Best Breast Cancer Hospital in Bangalore for Advanced Cancer Care
Home Breast cancer is one of the most commonly diagnosed cancers, and early, specialized treatment plays a crucial role in successful outcomes. Choosing the best breast cancer hospital in Bangalore ensures access to advanced medical expertise, accurate diagnosis, and comprehensive treatment planning. At Healius Cancer & Hematology, Bangalore, we provide evidence-based, patient-focused breast cancer care with an emphasis on precision, safety, and long-term well-being. Understanding Breast Cancer Breast cancer can present in various forms and stages. Common symptoms may include: A lump or thickening in the breast or underarm Changes in breast shape or skin texture Nipple discharge or inversion Persistent breast pain Timely evaluation by an oncology specialist is essential for accurate diagnosis and effective treatment. Why Healius Is a Trusted Breast Cancer Hospital in Bangalore 1. Accurate Diagnosis and Staging At Healius, breast cancer evaluation involves: Detailed clinical examination Imaging and pathology coordination Precise cancer staging to guide treatment decisions Early and accurate diagnosis improves treatment success and outcomes. 2. Personalized Breast Cancer Treatment Planning Every breast cancer case is unique. Treatment plans are individualized based on: Cancer type and stage Tumor biology and patient health International oncology treatment protocols This ensures optimal treatment effectiveness with minimized side effects. 3. Multidisciplinary Breast Cancer Care Effective breast cancer treatment requires coordinated expertise. Care at Healius integrates: Medical oncology Surgical oncology coordination Hematology and supportive oncology services This multidisciplinary approach supports continuity of care at every stage. 4. Focus on Quality of Life and Survivorship Beyond cancer treatment, Healius emphasizes: Symptom management and supportive care Emotional and psychological support Long-term follow-up and survivorship planning Our goal is to support patients not only through treatment, but also through recovery and beyond. Breast Cancer Services Available at Healius Bangalore Healius Cancer & Hematology provides comprehensive care pathways for: Early-stage and advanced breast cancer Diagnostic and staging services Medical oncology and chemotherapy Post-treatment monitoring and follow-up All care is delivered with transparency, compassion, and clinical excellence. Patient-Centered Breast Cancer Care in Bangalore A breast cancer diagnosis can be emotionally challenging. At Healius, patients receive: Clear communication about diagnosis and treatment options Supportive counseling and care coordination Continuous follow-up for long-term health monitoring We strive to ensure that every patient feels informed, supported, and empowered. Why Patients Choose Healius Cancer & Hematology Patients searching for the *best breast cancer hospital in Bangalore* trust Healius because of our: Specialized oncology focus Evidence-based and ethical care practices Multidisciplinary care model Compassionate, patient-first approach Choosing the Right Breast Cancer Hospital in Bangalore When selecting a hospital, patients should consider: Experience in breast oncology Availability of comprehensive cancer services Commitment to follow-up and survivorship care At Healius Cancer & Hematology, Bangalore, we are committed to delivering reliable, advanced, and patient-focused breast cancer care.
Best Hospital for Head and Neck Surgeon in Bangalore

Home Head and neck cancers affect critical areas such as the mouth, throat, voice box, thyroid, salivary glands, and facial structures. Choosing the *best hospital for a head and neck surgeon in Bangalore* is essential to ensure accurate diagnosis, safe surgery, and long-term functional recovery. At Healius Cancer & Hematology, Bangalore, we provide specialized, coordinated head and neck oncology care with a strong focus on clinical precision, patient safety, and quality of life. Understanding Head and Neck Cancer Care Head and neck cancer treatment often requires complex decision-making due to the involvement of vital organs responsible for speech, swallowing, breathing, and appearance. Effective management demands: Early and accurate diagnosis Specialized surgical expertise Multidisciplinary oncology collaboration Healius delivers structured head and neck cancer care aligned with international clinical standards. Why Healius Is a Trusted Hospital for Head and Neck Surgery in Bangalore 1. Comprehensive Diagnostic Evaluation Patients undergo detailed assessments including: Clinical examination Imaging and pathology coordination Cancer staging and risk assessment This ensures the most appropriate treatment pathway is selected. 2. Personalized Surgical Oncology Planning Head and neck cancer surgeries are planned with attention to: Tumor location and extent Functional preservation (speech and swallowing) Patient health and recovery goals Every treatment plan is individualized. 3. Multidisciplinary Head and Neck Oncology Approach Care at Healius integrates: Surgical oncology coordination Medical oncology support Hematology and supportive care services This collaborative approach improves treatment accuracy and outcomes. 4. Focus on Functional Outcomes and Recovery Beyond tumor removal, we emphasize: Post-surgical rehabilitation guidance Pain and symptom management Nutritional and supportive care coordination Our goal is not only cancer control, but also long-term quality of life. Head and Neck Cancer Services Supported at Healius Bangalore Healius Cancer & Hematology supports comprehensive care pathways for: Oral cavity cancers Throat and laryngeal cancers Thyroid and salivary gland tumors Diagnostic and staging surgical procedures All care is delivered with transparency, empathy, and clinical integrity. Patient-Centered Head and Neck Cancer Care We recognize the emotional and physical challenges faced by patients with head and neck cancers. At Healius, patients receive: Clear explanation of diagnosis and treatment options Emotional support and counseling Structured follow-up and survivorship care Our patient-first approach ensures dignity and trust throughout the treatment journey. — Why Patients Choose Healius Cancer & Hematology Patients looking for the best hospital for head and neck surgeon in Bangalore trust Healius because of our: Specialized oncology focus Ethical and evidence-based treatment protocols Experienced, multidisciplinary care team Compassionate patient engagement Choosing the Right Head and Neck Cancer Hospital in Bangalore When selecting a hospital, patients should consider: Experience in head and neck oncology Access to comprehensive cancer services Commitment to long-term follow-up and care At *Healius Cancer & Hematology, Bangalore*, we are dedicated to providing reliable, advanced, and compassionate head and neck cancer care.
Best Hospital for Head and Neck Surgeon in Bangalore

Home Head and neck cancers affect critical areas such as the mouth, throat, voice box, thyroid, salivary glands, and facial structures. Choosing the *best hospital for a head and neck surgeon in Bangalore* is essential to ensure accurate diagnosis, safe surgery, and long-term functional recovery. At Healius Cancer & Hematology, Bangalore, we provide specialized, coordinated head and neck oncology care with a strong focus on clinical precision, patient safety, and quality of life. Understanding Head and Neck Cancer Care Head and neck cancer treatment often requires complex decision-making due to the involvement of vital organs responsible for speech, swallowing, breathing, and appearance. Effective management demands: Early and accurate diagnosis Specialized surgical expertise Multidisciplinary oncology collaboration Healius delivers structured head and neck cancer care aligned with international clinical standards. Why Healius Is a Trusted Hospital for Head and Neck Surgery in Bangalore 1. Comprehensive Diagnostic Evaluation Patients undergo detailed assessments including: Clinical examination Imaging and pathology coordination Cancer staging and risk assessment This ensures the most appropriate treatment pathway is selected. 2. Personalized Surgical Oncology Planning Head and neck cancer surgeries are planned with attention to: Tumor location and extent Functional preservation (speech and swallowing) Patient health and recovery goals Every treatment plan is individualized. 3. Multidisciplinary Head and Neck Oncology Approach Care at Healius integrates: Surgical oncology coordination Medical oncology support Hematology and supportive care services This collaborative approach improves treatment accuracy and outcomes. 4. Focus on Functional Outcomes and Recovery Beyond tumor removal, we emphasize: Post-surgical rehabilitation guidance Pain and symptom management Nutritional and supportive care coordination Our goal is not only cancer control, but also long-term quality of life. Head and Neck Cancer Services Supported at Healius Bangalore Healius Cancer & Hematology supports comprehensive care pathways for: Oral cavity cancers Throat and laryngeal cancers Thyroid and salivary gland tumors Diagnostic and staging surgical procedures All care is delivered with transparency, empathy, and clinical integrity. Patient-Centered Head and Neck Cancer Care We recognize the emotional and physical challenges faced by patients with head and neck cancers. At Healius, patients receive: Clear explanation of diagnosis and treatment options Emotional support and counseling Structured follow-up and survivorship care Our patient-first approach ensures dignity and trust throughout the treatment journey. — Why Patients Choose Healius Cancer & Hematology Patients looking for the best hospital for head and neck surgeon in Bangalore trust Healius because of our: Specialized oncology focus Ethical and evidence-based treatment protocols Experienced, multidisciplinary care team Compassionate patient engagement Choosing the Right Head and Neck Cancer Hospital in Bangalore When selecting a hospital, patients should consider: Experience in head and neck oncology Access to comprehensive cancer services Commitment to long-term follow-up and care At *Healius Cancer & Hematology, Bangalore*, we are dedicated to providing reliable, advanced, and compassionate head and neck cancer care.
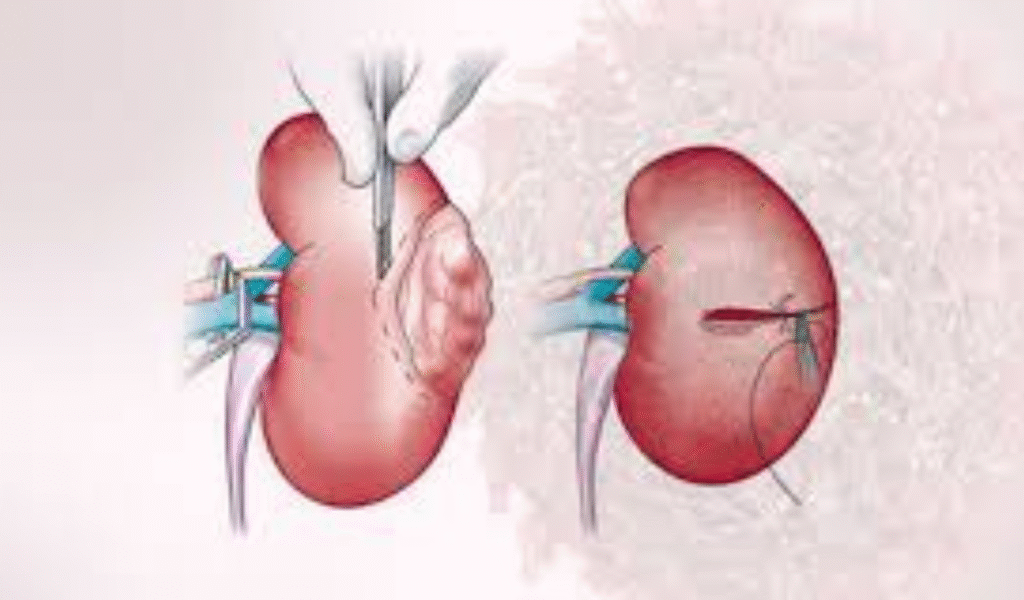
Find the Best Surgical Oncologist in Bangalore for Cancer Surgery
Home A cancer diagnosis can be overwhelming, and choosing the right surgical oncologist in Bangalore is one of the most important decisions in a patient’s treatment journey. Cancer surgery often plays a critical role in diagnosis, staging, treatment, and long-term outcomes. At Healius Cancer & Hematology, Bangalore, we provide expert-led, evidence-based surgical oncology care focused on safety, precision, and patient well-being. What Is Surgical Oncology? Surgical oncology is a specialized field of cancer care that focuses on the surgical management of tumors. This includes: Cancer diagnosis and biopsy procedures Removal of solid tumors Lymph node assessment Cancer staging and reconstruction planning An experienced surgical oncologist ensures that cancer is removed effectively while preserving organ function and quality of life. Why Choosing the Best Surgical Oncologist in Bangalore Matters Cancer surgery requires more than technical skill. It demands deep clinical judgment, multidisciplinary coordination, and patient-centered decision-making. At Healius Cancer & Hematology, our surgical oncology approach emphasizes: 1. Accurate Cancer Evaluation Every patient undergoes thorough clinical and diagnostic assessment to determine: Cancer type and stage Surgical feasibility Best possible treatment sequence 2. Personalized Surgical Treatment Planning No two cancers are the same. Surgical plans are customized based on: Tumor location and extent Patient health and recovery considerations International oncology guidelines 3. Multidisciplinary Cancer Care Surgical oncology at Healius is integrated with: Medical oncology Hematology Diagnostic and supportive care teams This ensures continuity of care before and after surgery. 4. Focus on Safety and Recovery Our cancer surgery protocols prioritize: Minimally invasive approaches where appropriate Reduced surgical complications Faster recovery and post-operative support Types of Cancer Surgery Supported at Healius Bangalore Healius Cancer & Hematology supports surgical oncology care as part of a coordinated treatment pathway for various cancers, including: Solid tumors requiring surgical intervention Diagnostic and staging procedures Post-surgical oncology follow-up and monitoring All surgical decisions are made with patient consent, clarity, and transparency. Patient-Centered Cancer Surgery Care in Bangalore We understand that cancer surgery is both a medical and emotional experience. At Healius, patients benefit from: Clear explanation of surgical options Pre- and post-surgery counseling Pain management and recovery guidance Long-term follow-up and survivorship care Our goal is to help patients feel informed, supported, and confident at every stage. Why Patients Trust Healius Cancer & Hematology Patients searching for the *best surgical oncologist in Bangalore* choose Healius because of our: Commitment to ethical and evidence-based cancer care Experienced oncology team Personalized treatment planning Compassionate, patient-first philosophy How to Choose the Right Surgical Oncologist in Bangalore When selecting a cancer surgeon, patients should consider: Experience in treating specific cancer types Clear communication and transparency Access to comprehensive oncology services At Healius Cancer & Hematology, Bangalore, we are dedicated to delivering trusted surgical oncology care aligned with global clinical standards.
Top Oncologist Center in Bangalore for Advanced Cancer Treatment
Home When it comes to cancer care, choosing the Right oncologist center in Bangalore can make a critical difference in treatment outcomes and quality of life. Patients and families seek not only advanced medical expertise, but also trust, transparency, and compassionate support throughout the cancer journey. At Healius Cancer & Hematology, Bangalore*, we are committed to delivering evidence-based, patient-centric cancer care that meets global clinical standards while remaining accessible and personalized. What Defines a Top Oncologist Center in Bangalore? A leading cancer treatment center is characterized by more than infrastructure alone. At Healius, our approach aligns with the highest benchmarks of oncology care: 1. Comprehensive Cancer Diagnosis Accurate diagnosis is the foundation of effective treatment. Our center provides: Advanced imaging and pathology Molecular and genetic testing (where indicated) Precise cancer staging for individualized treatment planning 2. Multidisciplinary Oncology Expertise Cancer treatment requires collaboration. Patients at Healius benefit from coordinated care involving: Medical oncologists Hematologists Radiation and surgical oncology coordination Oncology nursing and supportive care teams 3. Personalized Cancer Treatment Plans Every cancer is unique. Treatment protocols are tailored based on: Cancer type and stage Patient health status and preferences International oncology guidelines 4. Advanced Chemotherapy & Hematology Services We specialize in: Medical oncology treatments Hematological malignancies (leukemia, lymphoma, myeloma) Day-care chemotherapy with strict safety protocols 5. Patient-Centered Cancer Care We understand that cancer affects more than the body. Our care philosophy emphasizes: Clear communication and counseling Emotional and psychological support Symptom management and quality-of-life care 6. Continuity of Care & Long-Term Follow-Up Cancer care does not end with treatment. We provide: Survivorship care plans Regular monitoring and follow-ups Management of treatment-related side effects Why Patients Choose Healius Cancer & Hematology in Bangalore Patients searching for the best oncologist center in Bangalore trust Healius because we combine: Clinical excellence Ethical, transparent medical practices Compassionate patient engagement Convenient access to specialized oncology services within Bangalore Our goal is to ensure that every patient receives timely, accurate, and empathetic cancer care close to home. Cancer Treatment Services Available in Bangalore at Healius Medical Oncology Hematology & Blood Disorders Chemotherapy Administration Cancer Diagnostics & Monitoring Supportive & Palliative Oncology Care Choosing the Right Oncologist in Bangalore Selecting a cancer specialist is a deeply personal decision. Patients should look for: Experience in treating specific cancer types Clear communication and treatment transparency Access to comprehensive oncology services
Leukemia & Lymphoma in Children vs. Adults: What You Need to Know

Home Leukemia and lymphoma are two of the most common types of blood cancers. While they can occur at any age, the way these diseases present and progress in children vs. adults often differs. Understanding these differences is key to early detection and effective treatment. At Healius Cancer & Hematology Clinics, Bangalore, we provide comprehensive care including blood cancer treatment in Bangalore, chemotherapy at economical cost, and radiation therapy in Bangalore to support patients at every stage of their journey. Causes & Risk Factors Though the exact causes of leukemia and lymphoma are not always known, several risk factors have been identified: Genetic predisposition – Family history of blood cancers increases the risk. Weakened immune system – Conditions like HIV or immune-suppressing treatments may lead to higher vulnerability. Environmental exposure – Prolonged exposure to radiation or harmful chemicals can trigger changes in blood cells. Age-related factors – Certain leukemias are more common in children (like acute lymphoblastic leukemia), while others are seen more in adults (like chronic lymphocytic leukemia). Symptoms to Watch For The symptoms may vary in children and adults, but some common warning signs include: Persistent fatigue and weakness – Low red blood cells cause anemia and constant tiredness. Unexplained fever and frequent infections – A weak immune system leads to repeated illness. Swollen lymph nodes or abdomen – Enlarged nodes or spleen can indicate lymphoma or leukemia progression. Easy bruising or bleeding – Platelet deficiency causes nosebleeds, gum bleeding, or unusual bruises. If you notice these symptoms in yourself or your child, seek specialized hematology consultation in Bangalore immediately. Treatment Options at Healius At Healius Cancer & Hematology Clinics, we offer advanced yet affordable treatments tailored for both children and adults: Chemotherapy at economical cost – Targeted medications to destroy cancer cells while minimizing side effects. Radiation therapy in Bangalore – Advanced technology to treat lymphomas effectively and safely. Immunotherapy & Targeted Therapy – Modern approaches to boost the immune system and attack only cancerous cells. Bone Marrow Transplant referrals & support – For cases where intensive treatment is required. Why Choose Healius? Expert Oncologists & Hematologists led by Dr. Mangesh Kamath with vast experience in blood cancer treatment. Affordable care with chemotherapy at economical cost and accessible treatment plans. Personalized approach for children and adults with age-specific treatment protocols. Comprehensive support including nutrition counseling, rehabilitation, and caregiver guidance. At Healius, we combine compassionate care with world-class medical expertise to give patients the best chance of recovery. Contact Us – Begin the Journey of Healing Location: Healius Cancer & Hematology Clinics, Banashankari 2nd stage, BangaloreContact: +91 9900613143 Website: www.healiuscancerhematology.com If you or your loved one is looking for blood cancer treatment in Bangalore, trust Healius for advanced care, affordable treatment options, and expert guidance. Conclusion Early detection and timely treatment save lives. This Leukemia & Lymphoma Awareness Month, let’s spread awareness and give hope to those fighting blood cancers.
Vaccines and Screening for Women’s Cancers

Home The word “cancer” often brings fear. But today, we have vaccines that can help prevent some cancers. One of the most important is the HPV vaccine, which protects against human papillomavirus (HPV) – a common sexually transmitted virus. Nearly 50% of sexually active people are exposed to HPV at some point. While most infections go away on their own, some high-risk types can cause cancers of the cervix, vagina, vulva, anus, penis, and even parts of the throat. 📊 Gynaecological Cancers in India – At a Glance 🧬 Cervical Cancer → ~1,00,000 new cases every year → 50,000–60,000 deaths 🧬 Ovarian Cancer → ~45,000 new cases annually 🧬 Endometrial (Uterine) Cancer → ~20,000+ cases, rising steadily 👉 Most of these cancers are detected late, making prevention and early detection very important. Why Vaccination Matters HPV vaccine prevents most cervical cancers and some other HPV-related cancers. Vaccination at the right age can reduce cervical cancer in India by 85–90%. Research is ongoing for vaccines against ovarian and uterine cancers. HPV Vaccine – A Proven Shield Protects against high-risk HPV strains (16 & 18). Best for girls and boys aged 9–14; can be given up to 26 years (sometimes till 45). Reduces risk of cancers of cervix, vulva, vagina, anus, penis, and throat. Safe, effective, and long-lasting. New Vaccines in Development OvarianVax – BRCA1/2 gene vaccines – for women at high risk of breast and ovarian cancer. Other therapeutic vaccines – p53, HER2, WT1 (target proteins in ovarian/uterine cancers). Still in trial phase, not available in routine practice. Types of Vaccines Type Purpose Examples Status Preventive Stops cancer before it starts HPV vaccines (Gardasil, Cervarix, Cervavac) ✅ Approved & available Therapeutic Helps fight existing cancer BRCA1/2, p53, HER2, WT1 vaccines 🔬 In research 💡 “Your Questions, Answered” 💡 Can married women take HPV vaccine? Yes, up to 26 years (sometimes till 45).💡 Will vaccines cure cancer? No, HPV vaccine prevents infection. Others are in trials.💡 Do vaccinated women still need Pap tests? Yes, because not all risks are covered.💡 Are BRCA vaccines available in India? Not yet – only in research. September is Gynaecological Cancer Awareness Month 🌸 At Healius Cancer and Haematology Clinics, you can: Get a Free Consultation with cancer specialists Do a Pap smear test for early detection Join our HPV Vaccine Drive to protect yourself and your family ✅ Final NoteGynaecological cancers affect lakhs of women in India every year. The HPV vaccine and regular screening are powerful tools to prevent cervical cancer, while new vaccines offer hope for ovarian and uterine cancers. At Healius Cancer and Haematology Clinics, guided by Dr. Mangesh Kamath, women receive world-class, updated treatment and prevention strategies with a strong focus on patient care and awareness.
Chronic Lymphocytic Leukaemia (CLL): The Slow but Manageable Blood Cancer
Home Chronic Lymphocytic Leukaemia (CLL): The Slow but Manageable Blood Cancer 🩸 What is CLL?Chronic Lymphocytic Leukaemia (CLL) is a type of blood and bone marrow cancer where the body makes too many abnormal white blood cells called lymphocytes. These cells look normal but do not work properly to fight infections. Over time, they build up in the blood, bone marrow, and lymph nodes, pushing out the healthy cells.Unlike aggressive leukaemia’s like AML or ALL, CLL is slow-growing. Many people live with CLL for years before needing treatment. In fact, some people may never need active therapy and are only monitored. 🌍 How Common is CLL?Globally, CLL is the most common adult leukaemia in Western countries.In India, it is less common compared to acute leukaemia’s (ALL and AML), but the number of cases is slowly increasing as life expectancy improves.CLL usually affects older adults, especially above 60 years.Rarely seen in young people or children.Men are affected more than women. ⚠️ Risk Factors and CausesThe exact cause of CLL is not known. But certain risk factors make it more likely:Older age – common after 55–60 yearsFamily history – risk is higher if a close relative has CLL or another blood cancerGender – men have slightly higher chancesGenetic changes – mutations in TP53, deletion of chromosome 17p, and IGHV gene status are linked to aggressive diseaseEnvironmental exposure – contact with pesticides, fertilisers, and industrial chemicals (studies ongoing)👉 CLL is not contagious and is not caused by lifestyle or diet. 🔍 Common Symptoms of CLLMany patients are diagnosed during a routine blood test without any symptoms. When present, symptoms may include:Swollen lymph nodes in the neck, armpits, or groinFatigue and weaknessFrequent infectionsFever or night sweatsUnexplained weight lossEnlarged spleen or liver (felt as fullness in abdomen)Easy bruising or bleeding (in later stages) 🧪 How is CLL Diagnosed?Blood tests (CBC): Show high lymphocyte count.Flow cytometry: Identifies abnormal lymphocytes.Bone marrow biopsy: Sometimes needed for confirmation.Genetic tests: Detect mutations like del(17p), TP53, and IGHV – important for risk assessment. 🎯 Risk Stratification in CLLCLL does not behave the same way in every patient. Some people live for decades without treatment, while others need immediate therapy. Risk stratification helps doctors decide the best approach.🔹 Risk Stratification Systems in CLL:Rai Staging (USA):Stage 0 → only high lymphocyte count (low risk)Stage I–II → lymph nodes, spleen, or liver enlarged (intermediate risk)Stage III–IV → anaemia or low platelets (high risk)Binet Staging (Europe):Stage A → 3 or fewer lymph node areas involvedStage B → more than 3 lymph node areas involvedStage C → anaemia or low platelets presentGenetic & Molecular Markers:Favourable: Mutated IGHV, normal chromosomesUnfavourable: TP53 mutation, 17p deletion, unmutated IGHVOther factors:Lymphocyte doubling time (LDT): Faster growth = higher riskBeta-2 microglobulin levels: High levels linked to aggressive disease👉 These risk groups guide whether a patient should be on watch & wait, given tablets, or considered for advanced therapies. 💊 Treatment Options for CLL1. Watchful Waiting (Active Surveillance)If no symptoms and blood counts are stable, immediate treatment is not needed.Regular check-ups every 3–6 months.This avoids unnecessary side effects of treatment.2. Targeted TherapyTablets like Ibrutinib, Acalabrutinib, Zanubrutinib (BTK inhibitors) block signals that CLL cells need to grow.Venetoclax helps kill cancer cells by targeting survival proteins.Often better tolerated than chemotherapy.3. Chemo-ImmunotherapyCombination of chemotherapy drugs (Fludarabine, Cyclophosphamide) with monoclonal antibodies (Rituximab).Still used in younger patients with good-risk genetics.4. Monoclonal AntibodiesDrugs like Rituximab, Obinutuzumab, Ofatumumab attach to CLL cells and help the immune system destroy them.5. Stem Cell TransplantRarely done today. Considered for young patients with very high-risk or resistant CLL. 🚀 Recent Advances in CLL TreatmentNext-generation BTK inhibitors (like Acalabrutinib, Zanubrutinib) are safer and more effective.Fixed-duration therapy with Venetoclax + Obinutuzumab offers deep remission without lifelong treatment.Genetic testing is now routine in deciding treatment plans.CAR-T cell therapy is being explored in trials for relapsed CLL. 📊 CLL vs Other Leukaemias – A Simple ComparisonFeatureCLLCMLALLAMLProgressionSlow (chronic)Slow (chronic)Fast (acute)Fast (acute)Typical Age>60 yrs40–60 yrsChildren & young adultsMostly adults, esp. >60 yrsCells InvolvedLymphocytesMyeloid cellsImmature lymphoblastsImmature myeloid cellsSymptomsOften none early; enlarged nodes, fatigueFatigue, splenomegaly, high WBCFever, bleeding, bone painFatigue, bleeding, infectionsTreatmentWatchful waiting, targeted therapy, antibodiesTKIs (Imatinib, etc.), sometimes transplantChemotherapy, targeted therapy, immunotherapyIntensive chemo, transplantCurabilityUsually controlled for years; remission possibleExcellent long-term control with TKIsHigh cure rates, esp. in childrenCurable with aggressive therapy but relapse risk exists 🌈 Living with CLL: A Message of ReassuranceCLL is often called a “chronic” cancer, meaning it can be controlled long-term. Many patients live a normal lifespan, especially with today’s advanced therapies. For many, CLL becomes a condition that is managed like diabetes or hypertension rather than a life-ending disease.Regular follow-up, timely treatment when needed, and support from family and healthcare teams make a huge difference. ❤️ Final Thoughts From Healius Cancer and Haematology ClinicsAt Healius Cancer and Haematology Clinics, we understand the anxiety that comes with a diagnosis of CLL. The good news is that treatment has advanced tremendously—from chemotherapy to highly effective targeted therapies that give excellent quality of life.Under the guidance of Dr. Mangesh Kamath, our team provides:Personalised treatment plans based on your risk profileAccess to the latest targeted medicinesHolistic care including emotional and family support👉 Remember: CLL is not the end. With modern science, it is a journey that can be lived with hope, strength, and dignity.
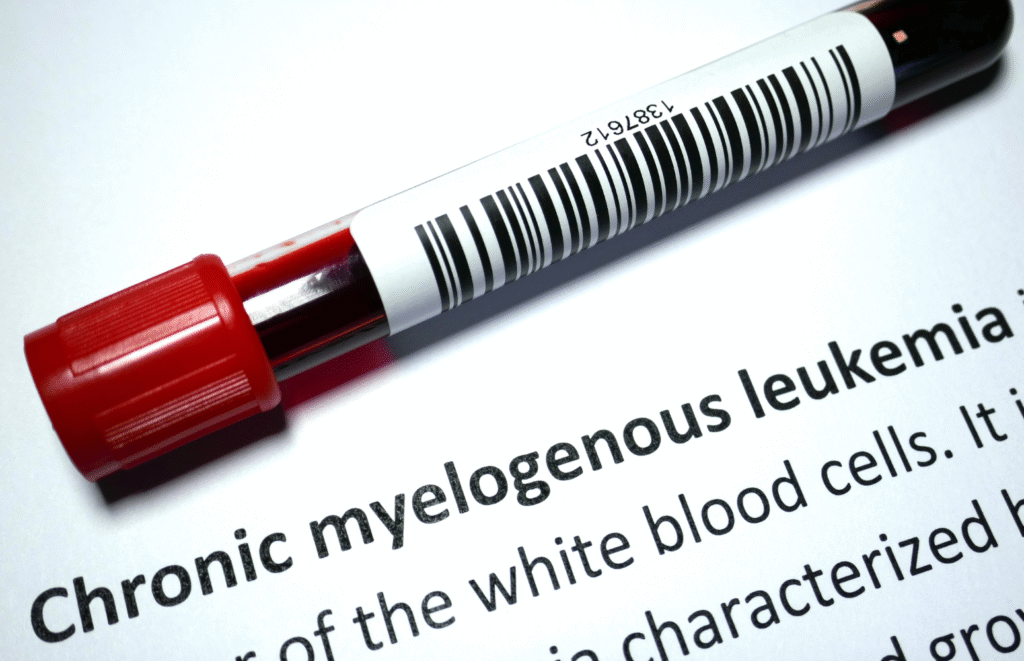
Breaking Down Chronic Myeloid Leukaemia: Your Guide to Understanding and Beating the Disease
Home Chronic Myeloid Leukaemia, commonly known as CML, is a type of blood cancer that starts in the bone marrow—the soft tissue inside bones where blood cells are made. CML mainly affects a group of white blood cells called myeloid cells, which normally help fight infections. But in CML, these cells grow uncontrollably and do not function as they should.Global and Indian PrevalenceAccording to the GLOBOCAN 2020 data, leukaemia accounts for over 474,000 new cases and 311,000 deaths globally each year. Among these, CML represents about 15–20% of adult leukaemia cases.In India, CML is the most common adult leukaemia, making up around 30–60% of adult cases depending on the region. It is much rarer in children, but when it occurs, it usually behaves more aggressively than in adults. What Causes CML?CML is not inherited. It happens due to a genetic change in the blood-forming cells. Almost all people with CML have a specific genetic abnormality called the Philadelphia chromosome, which creates a faulty gene called BCR-ABL1. This gene tells the body to produce a protein that makes abnormal cells grow too fast.Risk FactorsCML does not usually have clear lifestyle-related risk factors like smoking or diet. However, a few things may slightly increase the risk:Exposure to high doses of radiation (such as during a nuclear accident)Age – It is more common in adults over 50Gender – Men are slightly more affected than womenIt is important to know that for most people, there is no clear reason why they develop CML.Signs and SymptomsIn the early (chronic) phase, many people do not feel sick and are diagnosed during routine blood tests. As the disease progresses, symptoms may appear, such as:Fatigue or weaknessUnexplained weight lossNight sweatsFeverPain or fullness under the ribs (due to an enlarged spleen) How is CML Diagnosed?A Complete Blood Count (CBC) is usually the first clue. If the white blood cell count is abnormally high, further tests like bone marrow biopsy, Philadelphia chromosome testing, or BCR-ABL1 gene testing are done to confirm the diagnosis.Phases of CMLCML progresses in three phases:Chronic Phase – Most patients are diagnosed here. Symptoms are mild or absent.Accelerated Phase – The disease becomes more active, with more abnormal cells.Blast Crisis – The disease behaves like acute leukaemia and is harder to treat. Risk Stratification in CML: Why It MattersWhen someone is diagnosed with CML, doctors do not just look at the blood counts and genes—they also try to estimate how aggressive the disease might be. This process is called risk stratification.What Are the Risk Stratification Scores in CML?Doctors use special scoring systems at the time of diagnosis to estimate how fast the CML may progress. This helps decide the intensity of treatment and monitoring. The most used risk scores include:🔹 Sokal ScoreOne of the oldest and most widely used tools. It considers:Age at diagnosisSize of the spleenPlatelet countPercentage of blast cells (immature white cells) in the bloodPatients are classified into:Low riskIntermediate riskHigh risk🔹 Hasford Score (Euro Score)An update to the Sokal score, it includes:AgeSpleen sizePlatelet countBlast, eosinophil, and basophil percentagesThis score also categorizes patients into low, intermediate, or high risk. 🔹 EUTOS ScoreA simpler model that mainly uses:Spleen sizeBasophil countThis score helps predict early response to treatment, especially in patients receiving tyrosine kinase inhibitors (TKIs).🔹 ELTS Score (EUTOS Long-Term Survival)This newer score focuses on predicting long-term survival, rather than just early response. It includes:AgeSpleen sizePlatelet countBlast percentageIt is currently one of the most preferred risk tools for newly diagnosed CML patients.Why Should You Care About These Scores?While the names and numbers may sound technical, these scores help your doctor:Choose the best drug for your specific risk categoryEstimate how closely you should be monitoredDecide whether more aggressive treatment (like a transplant) might be needed laterMost importantly, they allow your care team to personalize your treatment plan to give you the best possible outcome.Treatment OptionsThanks to medical advances, CML is now considered a manageable chronic condition, especially when diagnosed in the chronic phase.1. Targeted Therapy (TKIs)The mainstay treatment for CML is Tyrosine Kinase Inhibitors (TKIs). These drugs block the BCR-ABL1 protein and stop the cancer from growing. Common TKIs include:ImatinibDasatinibNilotinibBosutinibPonatinibAsciminibMost patients take a TKI as tablets daily, often for life, but some may qualify for treatment-free remission if the disease stays under control for years.2. Bone Marrow or Stem Cell TransplantThis is usually reserved for patients who do not respond to TKIs or are in advanced stages. It is a more intense treatment with potential risks, but it can be curative.3. Chemotherapy or ImmunotherapyTraditional chemotherapy is rarely needed, but interferon-alpha, a type of immunotherapy, was used before TKIs and may still help in selected patients. Newer immunotherapy options are still under research for CML, including CAR T-cell therapy, but are not yet standard treatment.Recent Advances in TreatmentSecond- and third-generation TKIs are now available, offering options if the first drug stops working or causes side effects.Treatment-free remission (TFR) is becoming a reality for some patients. If a person has a deep, sustained response for years, they might be able to stop treatment under close monitoring.Molecular monitoring through PCR tests helps doctors track how well the treatment is working by measuring the level of BCR-ABL1 in the blood. Living with CMLRegular follow-ups are crucial. Blood tests and molecular tests help keep the disease in check.Side effects of TKIs can include fatigue, muscle cramps, and skin rashes—but many people tolerate them well.Mental health support is equally important. Learning to live with a lifelong illness can be emotionally challenging, and talking to a counsellor or support group can help. Can CML Be Prevented?Unfortunately, since the exact cause of CML is unknown in most cases, there are no proven preventive measures. However:Avoiding unnecessary radiation exposurePrompt health check-ups for symptomscan help in early detection and timely treatment. Final ThoughtsAt Healius Cancer and Haematology Clinics, we understand that a diagnosis of Chronic Myeloid Leukaemia (CML) can be overwhelming—not just for the patient, but for the entire family. But the good news is that CML is one of the most successfully treated forms of leukaemia today.
Acute Myeloid Leukaemia: Understanding the Disease of the Blood
Home Among the body fluids blood plays a major role in vital functioning of our body. It carries oxygen, nutrients to all organs and acts as a scavenger by carrying waste products to respective organs for further processing where they are removed from the body. The blood consists of four main components which are red blood cells, white blood cells, platelets, and plasma. These components are produced in the bone marrow which is the spongy tissue inside your bones. The myeloid stem cells originated from the bone marrow further differentiates into white blood cells, red cells, and platelets. When there is abnormal or uncontrolled production of these undifferentiated myeloid cells (called myeloblast) cause fast growing cancer of the bone marrow and blood known as Acute Myeloid Leukaemia. What Causes Acute Myeloid Leukaemia (AML)? AML is caused due to the changes that occur in our genes in the DNA of the Myeloid cells. Yet it is still unknown as to what triggers the change. However, there are few risk factors that increases the risk of AML which includes:Older Age – Acute myelogenous leukaemia is most common in adults age 65 and older.Gender – Global data shows men have about a 1.5 times higher risk of developing AML as compared to women. This could be due to higher exposure to like smoking, industrial chemicals and radiation in male dominated jobs and hormonal differences.Genetic Changes: Some people are born with gene mutations that make them more likely to develop AML later in life. Other mutations happen over time due to aging or environmental exposures. Previous Cancer Treatments: Chemotherapy and radiation, while life-saving, can sometimes damage bone marrow cells and trigger AML years later. Chemical Exposure: Long-term contact with chemicals like benzene (found in gasoline and industrial solvents) has been linked to AML. Blood Disorders: Conditions like myelodysplastic syndrome (MDS) can turn into AML if not treated early. Family History: Rare genetic conditions like Down syndrome increase AML risk. How Common Is AML? (Global & Indian Statistics)AML is more common in older adults, with most cases diagnosed after age 65. According to GLOBOCAN 2022 (a global cancer database): Worldwide: About 119,000 people are diagnosed with AML each year, and sadly, around 95,000 die from it. The survival rate is around 30% for adults, but younger patients often do better. In India: Roughly 6,000 to 8,000 new AML cases occur yearly. Many patients face delays in diagnosis due to lack of awareness, limited access to advanced tests, and high treatment costs. What Are the Symptoms of AML? Since AML affects blood cell production, symptoms often include: Extreme tiredness and weakness (due to low red blood cells). Frequent infections (because of a shortage of healthy white blood cells). Easy bruising or bleeding (such as nosebleeds or gum bleeding, due to low platelets). Bone pain (as leukemia cells build up in the marrow). Fever, night sweats, and unexplained weight loss.These symptoms can appear suddenly and worsen quickly, so seeing a doctor early is crucial. How Do Doctors Determine the Severity of AML? (Risk Stratification)Not all AML cases are the same—some are more aggressive than others. Doctors classify AML into low, intermediate, and high-risk categories based on: Genetic Testing: Certain gene changes (like FLT3 or NPM1 mutations) help predict how well treatment will work. Age & Overall Health: Younger, fitter patients usually respond better to strong chemotherapy. Response to Initial Treatment: If cancer cells disappear after the first round of chemo, chances of long-term survival improve. Why Does Risk Stratification Matter?Low-risk AML may be cured with chemotherapy alone. Intermediate-risk AML might need chemotherapy followed by a stem cell transplant. High-risk AML often requires stronger treatments, like targeted therapy or clinical trials. This personalized approach helps doctors choose the best treatment while avoiding unnecessary side effects. What Are the Treatment Options for AML?1. ChemotherapyThe standard first treatment is “7+3” chemotherapy—a combination of two drugs given over 7 days. This kills leukaemia cells but also affects healthy cells, causing side effects like hair loss, nausea, and low blood counts. 2. Targeted Therapy Newer drugs specifically attack cancer cells without harming normal cells as much. Examples include: FLT3 inhibitors (Gilteritinib, Midostaurin) for patients with FLT3 mutations. IDH inhibitors (Ivosidenib) for those with IDH1/2 mutations. 3. Stem Cell TransplantFor high-risk patients, a bone marrow transplant (from a donor) may be the best chance for a cure. However, it is a complex procedure with risks like infections and graft-versus-host disease (where donor cells attack the body). 4. Supportive Care Since AML weakens the immune system, patients often need: Blood transfusions (to replace red cells and platelets). Antibiotics (to prevent infections). Pain management (for bone pain). 5. Special Case: APL (A Highly Curable Subtype) A rare form of AML called acute promyelocytic leukemia (APL) is treated differently—with vitamin A-based drugs (ATRA) and arsenic trioxide, leading to cure rates above 90%. Hope for the Future While AML remains a serious disease, advances in genetic testing, targeted therapies, and immunotherapy are improving survival rates. Early diagnosis and access to specialized care are critical—especially in countries like India, where awareness and healthcare access vary widely. If you or a loved one experience persistent fatigue, infections, or unusual bleeding, consult a doctor promptly. With the right treatment, many AML patients can achieve remission and lead fulfilling lives.
