Ovarian Cancer: Navigating the Challenges of Late Diagnosis, Biomarker Limitations, and Tumor Heterogeneity
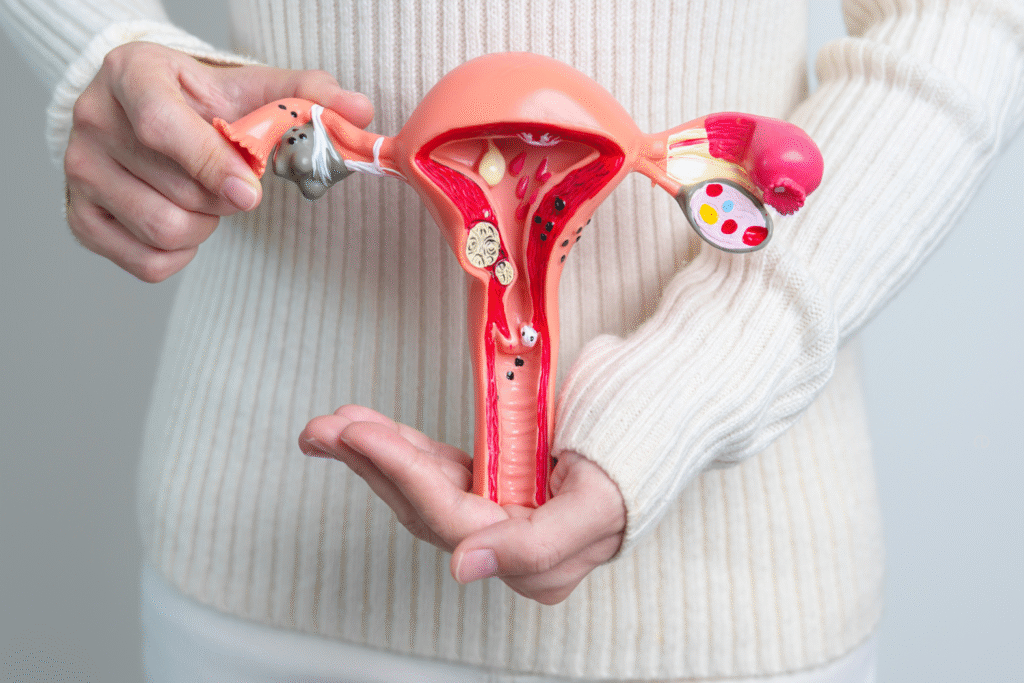
Home Ovarian cancer remains one of the most lethal gynaecologic malignancies, with a five-year survival rate of only ~50% for advanced-stage cases. Despite advances in treatment, significant challenges persist late diagnosis, inefficient biomarkers, and extreme tumour heterogeneity, each contributing to poor outcomes. Among these, late diagnosis is arguably the most formidable challenge, as it drastically limits treatment efficacy and survival. However, emerging research is paving the way for improved detection, personalized therapies, and novel treatment strategies. Late Diagnosis: The Biggest Hurdle in Ovarian Cancer Management Why Late Diagnosis is So Devastating ~70% of ovarian cancer cases are diagnosed at Stage III or IV, when the disease has already metastasized. No reliable screening test exists (unlike mammograms for breast cancer or Pap smears for cervical cancer). Symptoms (bloating, pelvic pain, urinary urgency) are non-specific, often leading to misdiagnosis (e.g., IBS, urinary infections). Consequences of Late Detection Limited surgical options: Optimal cytoreduction (tumour debulking) is harder in advanced disease. Higher chemoresistance risk: Late-stage tumours often develop resistance to platinum-based therapies. Poor survival rates: Early-stage (I/II) survival exceeds 90%, but late-stage survival drops to ~30%. Efforts to Improve Early Detection Liquid biopsies (circulating tumor DNA, exosome profiling) are under investigation. Multi-cancer early detection (MCED) tests are being explored, though none are yet FDA-approved for ovarian cancer. Awareness campaigns aim to educate on symptoms.Biomarker Limitations: The Challenge of Precision Medicine Current Biomarkers and Their Shortcomings CA-125: The most widely used biomarker, but non-specific (elevated in endometriosis, pregnancy, other cancers). HE4: Better specificity but still not definitive for early detection. HRD Testing: Helps identify PARP inhibitor responders, but 22% of high-grade serous ovarian cancers (HGSC) show spatial heterogeneity in HRD scores, leading to inconsistent results. Folate Receptor Alpha (FRα): Used for mirvetuximab soravtansine eligibility, but only ~35-40% of patients have sufficient FRα expression. Emerging Biomarkers Multi-omics profiling (genomics, proteomics, metabolomics) is identifying new signatures (e.g., FXYD6, linked to ferroptosis and immunotherapy resistance). Tumor microenvironment (TME) biomarkers (e.g., CD8+ T-cell infiltration) may predict immunotherapy response. Tumor Heterogeneity: A Major Barrier to Effective Treatment Types of Heterogeneity in Ovarian Cancer Spatial heterogeneity: Different tumour regions (e.g., ovary vs. omentum) show varying biomarker expression (e.g., PR, Ki67). Temporal heterogeneity: Recurrent tumours often evolve, acquiring new mutations (e.g., **BRCA reversion mutations** causing PARPi resistance). Molecular subtypes: High-grade serous (HGSC): Most common (~70%), highly aggressive, TP53 mutations. Low-grade serous (LGSC): Rare (~10%), younger patients, often KRAS/BRAF-mutated. Clear cell & endometrioid: Differ in chemosensitivity and molecular drivers. Impact on Treatment Chemotherapy resistance: Clonal evolution leads to subpopulations that evade treatment. Immunotherapy limitations: “Cold” tumours (low T-cell infiltration) respond poorly to checkpoint inhibitors. Current and Emerging Treatments to Overcome These Challenges Targeted Therapies PARP inhibitors (olaparib, niraparib): Effective in BRCA-mutated and HRD-positive tumours, but resistance remains a hurdle. Antibody-drug conjugates (mirvetuximab soravtansine): For FRα-positive platinum-resistant cases. MEK inhibitors (trametinib, binimetinib): Show promise in low-grade serous ovarian cancer (LGSC). Immunotherapy & Novel Approaches Combination therapies: PARPi + immunotherapy (e.g., pembrolizumab) are being tested to convert cold tumours to hot. Ferroptosis inducers: Targeting FXYD6 to trigger iron-dependent cell death. Adoptive cell therapy (CAR-T, TILs): Early-phase trials show potential in recurrent disease. Preventive Strategies Risk-reducing surgery: Salpingectomy (fallopian tube removal) and Oophorectomy (removal of ovaries) for BRCA carriers may prevent HGSOC. Genetic testing expansion: Only ~50% of ovarian cancer patients receive germline testing, missing hereditary risks (e.g., Lynch syndrome). Which Challenge is the Greatest? While biomarker limitations and tumour heterogeneity complicate treatment, late diagnosis remains the most critical challenge — without early detection, even the best therapies are less effective. However, advances in multi-omics profiling, liquid biopsies, and novel targeted agents are offering hope. The future of ovarian cancer management lies in: Better early detection tools (e.g., AI-driven imaging, blood-based assays). Comprehensive biomarker testing at diagnosis (HRD, FRα, BRCA). Personalized combination therapies to overcome resistance. With sustained research and advocacy (e.g., OCRA’s $6M funding in 2025), we may finally shift ovarian cancer from a silent killer to a manageable disease.
Understanding Mouth Cancer

Home Mouth cancer, also known as oral cancer, is a serious but treatable condition—especially when diagnosed early. At Healius Cancer & Hematology Clinics, we believe that awareness is the first step toward prevention and early intervention. In this blog, we break down the most important aspects of mouth cancer: its symptoms, causes, and early warning signs. What Is Mouth Cancer? Mouth cancer refers to cancer that develops in any part of the oral cavity, including the lips, tongue, cheeks, gums, roof of the mouth (palate), floor of the mouth, and throat. It usually begins in the squamous cells lining the mouth and can spread quickly if left untreated. Early Symptoms and Warning Signs Detecting mouth cancer early dramatically increases the chances of successful treatment. Be alert to the following warning signs: A persistent sore or ulcer that doesn’t heal within 2–3 weeks Red or white patches inside the mouth Unexplained bleeding in the mouth Lump or thickening in the cheek or neck Difficulty in swallowing, speaking, or moving the jaw Numbness or pain in the mouth or lips Persistent sore throat or a feeling of something stuck in the throat Sudden weight loss or voice changes If you notice any of these symptoms, it’s crucial to consult a cancer specialist without delay. What Causes Mouth Cancer? Several risk factors are associated with the development of mouth cancer: Tobacco use (smoking or chewing) – the leading cause Excessive alcohol consumption HPV infection (Human Papillomavirus) Poor oral hygiene and chronic irritation Exposure to the sun (for lip cancer) Diet low in fruits and vegetables Genetic predisposition At Healius Cancer & Hematology Clinics Bangalore, we emphasize both lifestyle modification and regular screenings to lower risk and catch potential problems early. Why Early Detection Matters When detected in the early stages, oral cancer can often be treated successfully with minimally invasive procedures. Unfortunately, many cases are diagnosed too late due to a lack of awareness. Healius Cancer & Hematology Clinics offer advanced head & neck cancer screenings, including oral cancer detection services led by experienced oncologists. Our comprehensive care ensures you get the right diagnosis, timely treatment, and compassionate support throughout your journey. How We Can Help Expert Team of Oncologists & Hematologists Advanced Diagnostic Tools & Biopsy Services Customized Treatment Plans: Surgery, Radiation, Chemotherapy & Immunotherapy Supportive Care for Nutrition, Pain Management, and Emotional Wellbeing Early Screening & Preventive Counselling Book a Consultation Whether you’re experiencing symptoms or want to schedule a routine screening, Healius Cancer & Hematology Clinics are here for you. Your health is in your hands—don’t wait. Book your appointment today at www.healiuscancerclinic.com or call us for immediate assistance +91 9900613143 Final Thoughts Mouth cancer doesn’t have to be a silent threat. With awareness, timely diagnosis, and expert care from Healius, it is possible to overcome it. Stay informed, stay vigilant—and spread the word.
Cancer Vaccines

Home Cancer vaccines represent a promising frontier in medical science, designed to either prevent cancer from developing or treat existing cancers by boosting the body’s immune response against cancer cells. Cancer vaccines offer a potential solution to the problems facing the field of oncology in the coming decade. These therapies benefit from economies of scale, simple administration, and may be more effective in earlier disease settings than later. Traditional vaccines aim to prevent or ameliorate infectious diseases through priming immune responses to exogenous antigens associated with given pathogens before a natural infection occurs. Similarly, cancer vaccines seek to induce an anti-tumor immunity using an appropriate delivery vector to prime responses to cancer antigens presented on the surface of tumour cells. Types of Cancer Vaccines Preventive (Prophylactic) Vaccines These are used to prevent cancer caused by viruses. HPV Vaccine: Protects against the human papillomavirus, which is linked to cervical, anal, throat, and other cancers. Hepatitis B Vaccine: Reduces the risk of liver cancer caused by Hepatitis B infection. Therapeutic Vaccines These are given to cancer patients to help the immune system recognize and destroy cancer cells. Research is ongoing for cancers like melanoma, prostate, and lung cancer. Therapeutic cancer vaccines can stop tumour from growing or spreading, destroys cancer cells still in the body after surgery and radiation therapy and also prevents relapse. Provenge (Sipuleucel-T): Approved for advanced prostate cancer. IMA901: Investigated for kidney cancer. Bacillus Calmette-Guerin (BCG): Approved for the treatment of early-stage cancer Nadofaragene firadonevec (Adstiladrin®): Approved for treatment of early-stage bladder cancers that have progressed despite BCG therapy. GVAX: A group of experimental vaccines for pancreatic and other cancers. Talimogene laherparepvec (T-VEC): An oncolytic virus-based vaccine approved for melanoma. Role in Cancer Prevention Early Intervention: Vaccines like HPV are most effective when administered before exposure to the virus, typically in adolescence. Reduced Burden: Mass vaccination programs can significantly reduce the incidence of certain cancers, particularly in women. Cost-effective: Long-term savings in healthcare costs by preventing cancers before they develop. Government of India’s Initiatives The Government of India is actively promoting cancer prevention through vaccination and awareness: Introduction of HPV Vaccine in National Immunization Programme In 2024, India included the indigenously developed HPV vaccine ‘CERVAVAC’ in the Universal Immunization Programme. This aims to reduce the incidence of cervical cancer, the second most common cancer among Indian women. This vaccine is advisable for girls who are above 9 yrs and women. Public Awareness Campaigns Nationwide campaigns promote awareness about the importance of early vaccination and routine screening. Collaboration with NGOs and digital platforms to reach rural and underserved communities. Screening and Early Detection Under Ayushman Bharat, health and wellness centre’s provide free screening for common cancers (oral, breast, and cervical). Integration of vaccine awareness in school health programs. Conclusion Cancer vaccines, especially the HPV and Hepatitis B vaccines, offer a significant opportunity to prevent cancers before they occur. With proactive steps like launching affordable vaccines and integrating them into public health schemes, India is paving the way for a cancer-free future.
Haemophilia
Home Haemophilia is often thought of as a “man’s disease,” but women and girls can have it too. Though less commonly diagnosed, females with haemophilia can experience significant bleeding issues that impact their daily lives. Understanding Haemophilia in Women Haemophilia is a genetic disorder where the blood doesn’t clot properly due to a deficiency in clotting factors. It’s linked to the X chromosome, meaning males (who have one X) are more likely to have severe symptoms. However, females (who have two X chromosomes) can also inherit the mutation. Traditionally, women were labelled as “carriers,” but many actually have mild, moderate, or even severe haemophilia. Symptoms in Women and Girls Women with haemophilia or low clotting factor levels may experience: Heavy and prolonged menstrual periods (menorrhagia) Frequent nosebleeds and easy bruising Excessive bleeding after childbirth, surgery, or dental work Joint and muscle bleeds, similar to male patients These symptoms are often overlooked or misdiagnosed, leading to delayed treatment. Challenges in Diagnosis and Care Many doctors still hesitate to diagnose women with haemophilia, instead labelling them as carriers. This medical bias means women often struggle for years before getting proper care. Additionally, female-specific issues—like menstrual bleeding—are sometimes dismissed as normal, even when they indicate an underlying bleeding disorder. Treatment and Management Women with haemophilia can benefit from the same treatments as men, including: Clotting factor replacement therapy Antifibrinolytic drugs (to reduce bleeding) Hormonal treatments to manage menstrual bleeding Preventive care to protect joints from damage Raising awareness is crucial for ensuring timely diagnosis and treatment for women and girls with haemophilia. No one should suffer due to outdated misconceptions. Breaking the Stigma The idea that “only men bleed” has been debunked—women and girls with haemophilia deserve recognition, care, and support. Advocacy groups, medical professionals, and patients are working together to push for better diagnosis, treatment, and awareness. It’s time to change the narrative: Women bleed too, and they deserve the care they need.
Breaking New Ground

Home Head and neck cancers affect thousands of individuals globally, but thanks to innovative research and clinical advancements, patients now have access to more effective, personalized, and less invasive treatment options. At Healius Cancer & Hematology Clinics, we are proud to be at the forefront of these changes, offering our patients access to the best head & neck cancer treatment in Bangalore, with a strong emphasis on quality care and advanced therapeutic techniques. 1. Neoadjuvant Immunotherapy: A Game Changer Traditionally, surgery was considered a primary treatment option for many head and neck cancers. However, neoadjuvant immunotherapy—administered before surgery—is reshaping this approach. This treatment stimulates the body’s immune system to attack cancer cells before any surgical intervention. Combinations like anti-PD1 therapy with CD40 agonist antibodies have shown remarkable results, improving immune response and potentially reducing the need for aggressive surgery. 2. Combination Immunotherapy: Strength in Unity Recent trials reveal that dual immunotherapy regimens offer better outcomes compared to monotherapy. By combining different immunotherapeutic agents, doctors are seeing higher response rates, longer remission periods, and improved patient resilience. This development is particularly promising for patients looking for head & neck cancer treatment without surgery. 3. Precision-Driven Targeted Therapies In a landmark move, the FDA has granted breakthrough therapy designation to the combination of petosemtamab and pembrolizumab. This duo is proving highly effective in treating recurrent or metastatic head and neck squamous cell carcinoma (HNSCC), especially in patients with specific biomarker expressions. At Healius, our personalized approach ensures that patients receive treatments tailored to their unique cancer profile. 4. Advanced Imaging: Better Vision, Better Outcomes Innovative CT scan techniques and imaging methods now enable oncologists to visualize tumors with greater accuracy. These technologies help in better diagnosis, staging, and surgical planning—ensuring that treatment strategies are more precise and minimally invasive. 5. Promising Clinical Trials We stay connected with emerging global clinical trials. Studies combining drugs like avelumab, cetuximab, and palbociclib are showing potential in controlling tumor growth while minimizing side effects. These trials point toward a future where non-surgical treatment options for head and neck cancer could become the norm for many patients. Why Choose Healius? At Healius Cancer & Hematology Clinics, we’re committed to providing affordable, world-class cancer care. Led by renowned oncologist Dr. Mangesh Kamath, we specialize in personalized treatment plans that incorporate the latest medical advances. Whether you’re looking for the best head & neck cancer treatment or exploring head & neck cancer treatment without surgery, our team is here to guide you every step of the way. Early detection, timely intervention, and expert care save lives. If you or your loved one is navigating a head or neck cancer diagnosis, reach out to us today. 📍 Healius Cancer & Hematology Clinics – Your Partner in Healing.
Breaking Myths About Lung Cancer

Home Lung cancer is one of the most common and misunderstood types of cancer. Myths and misconceptions often lead to fear, stigma, and delayed diagnosis. At Healius Cancer & Hematology Clinics, under the expert guidance of Dr. Mangesh Kamath, we strive to spread awareness, debunk myths, and provide advanced care for lung cancer patients. Myth 1: Only Smokers Get Lung Cancer Reality: While smoking is a significant risk factor, non-smokers can also develop lung cancer. Exposure to environmental pollutants, second-hand smoke, genetic factors, and occupational hazards like asbestos can contribute to the disease. Dr. Mangesh Kamath and his team at Healius Cancer & Hematology Clinics emphasize early screening for high-risk individuals, regardless of smoking history. Myth 2: Lung Cancer is Always Fatal Reality: Advances in medical technology and personalized treatment approaches have significantly improved survival rates. Early detection, targeted therapies, immunotherapy, and advanced surgical procedures have led to better outcomes. At Healius, Dr. Mangesh Kamath leads a multidisciplinary team offering state-of-the-art treatments tailored to each patient’s condition. Myth 3: If You Have No Symptoms, You Don’t Have Lung Cancer Reality: Lung cancer can remain asymptomatic in its early stages. Symptoms like persistent cough, shortness of breath, chest pain, unexplained weight loss, and fatigue often appear in later stages. This is why routine screenings, especially for high-risk individuals, are crucial. Healius Cancer & Hematology Clinics offer comprehensive screening programs to ensure early diagnosis and timely intervention. Myth 4: Lung Cancer Cannot Be Treated Effectively Reality: With the latest advancements in cancer treatment, lung cancer is treatable and manageable. Healius Cancer & Hematology Clinics provide cutting-edge treatments, including: Targeted Therapy – Personalized treatment based on genetic mutations. Immunotherapy – Boosting the immune system to fight cancer cells. Minimally Invasive Surgery – Reducing recovery time and complications. Radiation and Chemotherapy – For both early and advanced-stage lung cancer. Myth 5: Lung Cancer Treatment is the Same for Everyone Reality: No two lung cancer cases are the same. Each patient requires a personalized treatment plan, which is why Dr. Mangesh Kamath and his team focus on precision oncology. At Healius, we use genetic profiling and advanced diagnostic tools to create customized treatment strategies that yield the best results for every individual. Trust Healius Cancer & Hematology Clinics for Expert Lung Cancer Care At Healius Cancer & Hematology Clinics, we are dedicated to providing world-class lung cancer treatment with a patient-centric approach. Under the leadership of Dr. Mangesh Kamath, our goal is to offer the best possible care through advanced technology, expertise, and compassionate support. If you or a loved one are at risk or experiencing symptoms, don’t wait. Book a consultation at Healius today and take the first step toward better lung health. For more details, visit our website – www.healiuscancerhematology.com or contact us at +91 9900613143
Hereditary Colorectal Cancer Awareness

Home Colorectal cancer (CRC) can be inherited in 10-15% of cases. Hereditary colorectal cancer awareness in India is still low despite rising cases. Many cases go undiagnosed due to lack of genetic testing, limited awareness and social stigma around discussing cancer. Types of Hereditary CRC Lynch Syndrome (HNPCC): – Accounts for ~3% of CRC cases, caused by mutations in DNA mismatch repair genes such as MLH1, MHS2, MSH6 and PMS2. Familial Adenomatous Polyposis (FAP): – Resulting from the mutation of APC gene, causing hundreds to thousands of polyps in the colon, leading to near-certain CRC if untreated. MUTYH – associated Polyposis (MAP): – Caused by mutations in MUTYH gene. Peutz – Jeughers Syndrome: Associated with mutation in STK11 gene. Cowden Syndrome: Caused by mutations in PTEN gene. Juvenile Polyposis Syndrome: Associated with mutation in BMPR1A and SMAD4 gene. Additionally, recent advancements in molecular techniques have identified new genes involved in CRC predisposition, including RPS20, POLE, POLD1, AXIN2, NTLH1, RNF43 AND GREM1. Who is at Risk? Individuals with a family history of CRC, especially if diagnosed before age 50. Those with a personal or family history of polyps. People with Lynch syndrome or FAP mutations. Certain Early Detection & Prevention Screening: – Colonoscopies starting at age 40 (or earlier if family history is strong). Genetic Testing: – Recommended for families with multiple CRC cases. Lifestyle Changes: – A healthy diet, regular exercise, and avoiding smoking/alcohol can lower risk. Awareness & Action Educate families about genetic risks. Encourage genetic counseling for high-risk individuals. Promote early screening to prevent CRC development.
Cervical Cancer

Home Cervical cancer is one of the most preventable and treatable forms of cancer when detected early. Despite medical advancements, it remains a major health concern for women worldwide. At Healius Cancer & Hematology Clinics, we are committed to raising awareness, providing preventive solutions, and delivering state-of-the-art treatment for cervical cancer. Understanding Cervical Cancer Cervical cancer originates in the cervix, the lower part of the uterus that connects to the vagina. The primary cause of cervical cancer is persistent infection with high-risk human papillomavirus (HPV), a common virus transmitted through intimate contact. While HPV infections are usually cleared by the immune system, some high-risk strains can lead to cervical cancer over time. Symptoms to Watch For Early-stage cervical cancer often presents no symptoms, making regular screenings essential. However, as the disease progresses, women may experience: Abnormal vaginal bleeding (between periods, after intercourse, or post-menopause) Unusual vaginal discharge with a foul odor Pelvic pain or discomfort Pain during intercourse Prevention: The Power of Vaccination and Screening At Healius Cancer & Hematology Clinics, we emphasize early detection and prevention through: HPV Vaccination: The HPV vaccine effectively protects against the high-risk strains that cause cervical cancer. It is recommended for girls and young women before the onset of sexual activity but can also benefit older individuals. Regular Pap Smears & HPV Testing: A Pap smear detects precancerous changes in cervical cells, allowing for early intervention. HPV testing helps identify high-risk infections that may lead to cancer. Advanced Diagnosis and Treatment at Healius Cancer & Hematology Clinics If detected early, cervical cancer is highly treatable. At Healius Cancer & Hematology Clinics, we provide personalized treatment plans based on the stage of cancer and individual patient needs. Our multidisciplinary team offers: Minimally Invasive Surgery: For early-stage cases, procedures like LEEP (Loop Electrosurgical Excision Procedure) and cone biopsy can remove precancerous or cancerous cells. Radiation Therapy: High-energy radiation is used to destroy cancer cells, often in combination with chemotherapy. Targeted Therapy & Immunotherapy: Cutting-edge treatments designed to attack cancer cells while preserving healthy tissue. Chemotherapy: Effective for advanced stages, chemotherapy helps shrink tumors and manage symptoms. Why Choose Healius Cancer & Hematology Clinics? Expert Oncology Team: Our specialists bring years of experience in diagnosing and treating cervical cancer with precision and care. Advanced Technology: We utilize the latest medical advancements to ensure the best possible outcomes. Holistic Patient Support: From diagnosis to recovery, we offer compassionate care, psychological support, and wellness programs to enhance the healing journey. Awareness & Education: We conduct community outreach programs to spread awareness about HPV vaccination and early detection. Take Charge of Your Health Today! Cervical cancer is preventable and treatable when detected early. Stay proactive by scheduling your routine screening at Healius Cancer & Hematology Clinics. If you or a loved one has concerns about cervical cancer, our expert team is here to provide guidance, support, and world-class treatment. Book your appointment today and take a step towards a cancer-free future. For more information, visit our website – www.healiuscancerhematology.com or contact us at +91 9900613143
Breast Cancer

Home Breast cancer is the most common cancer among Indian women, with the cases steadily increasing. Breast cancer accounts for 27% of all female cancers in India, with cases projected to rise 170% by 2050. Mortality rates may increase 200%, and the five-year survival rate is 66.4%. In 2024, India recorded approximately 2,60,000 new breast cancer cases. In Karnataka, the total number of new cancer cases was 87,855, with breast cancer being the most prevalent among women. With this alarming increase in number of cases, let us understand the possible risks, nature and types of breast cancer and the possible treatments available and preventive measures. Risk Factors Family history of cancers who could be possible carriers of various pathogenic mutations. A recent indigene study shows about 40% cases of breast cancers could be hereditary in nature. Hormonal and reproductive factor: Early menstruation (before 12), late menopause (after 55), Late or no pregnancies, Hormone replacement therapy. Lifestyle and environmental factors including obesity, excessive alcohol consumption, smoking, radiation exposure, sedentary lifestyle, lack of proper diet, exposure to heavy metals, pesticides etc. Aging (higher risk after 50) Dense breast tissue (more glandular tissue than fatty tissue) Other breast conditions such as ADH, ALH, fibroadenomas with complex features, papillomas (small wart-like growths in milk ducts), Radial scars (star-shaped breast tissue formation) etc. LCIS, which is abnormal cell growth in the milk producing glands (lobules). Women with LCIS have a 7-12 times higher risk of invasive breast cancer. Types of Breast Cancer There are many types of breast cancer, and many different ways to describe them. It’s easy to get confused. A breast cancer’s type is determined by the specific cells in the breast that become cancer. Non-Invasive (In-situ) Breast Cancer – DCIS: Cancer cells in milk ducts but haven’t spread. Invasive Breast Cancer: Invasive Ductal Carcinoma – IDC – Most common type; spreads beyond milk ducts Invasive Lobular Carcinoma – ILC – starts in lobules, may spread. Triple Negative Breast Cancer (TNBC) – Lacks estrogen, progesterone, and HER2 receptors; aggressive and harder to treat. HER2-Positive Breast Cancer – Has high levels of HER2 protein, often aggressive but treatable. Inflammatory Breast Cancer (IBC) – Rare and aggressive, causes red, swollen breast. Paget’s Disease of the Breast – Affects the nipple and surrounding area. Treatment Options: Treatment depends on the type, stage, and patient’s overall health. 1. Surgery – Lumpectomy (removes tumor, keeps most of the breast) – Mastectomy (removes one or both breasts) 2. Radiation Therapy – Uses high-energy rays to kill cancer cells, often after surgery. 3. Chemotherapy – Uses drugs to destroy cancer cells, often before or after surgery. 4. Hormone Therapy – Blocks hormones like estrogen/progesterone that fuel cancer growth. 5. Targeted Therapy – Attacks specific cancer cell markers like HER2 (e.g., Herceptin). 6. Immunotherapy – Boosts immune system to fight cancer, mainly for TNBC. Prevention Strategies – Healthy Lifestyle: Exercise regularly, maintain a healthy weight, avoid smoking and limit alcohol. – Breastfeeding: May lower risk. – Regular Screening: Mammograms help detect early signs. – Genetic Testing & Risk-Reducing Measures: Consider if high risk (e.g., BRCA mutations). – Limit Hormone Therapy: Use the lowest effective dose for the shortest time if needed.
Childhood Leukemia

Home Childhood leukaemia, the most common cancer in children, accounts for about 30% of all paediatric cancers. Every year, almost 25,000 children in India are diagnosed with cancer, with nearly 9000 of them having leukaemia. It affects the blood and bone marrow, leading to abnormal white blood cell production. While much information is available, some lesser-known facts about its symptoms, causes, and treatment options remain unfamiliar to many. Uncommon Symptoms of Childhood leukaemia Most people recognize common symptoms like persistent fatigue, fever, and easy bruising, but there are some lesser-known signs that might be overlooked: 1. Changes in Eye Appearance – Some children develop white or bluish spots in the eyes due to leukaemia-related eye involvement.– Swelling around the eyes and sudden vision problems may also occur. 2. Prolonged Bone Pain Misdiagnosed as Growing Pains – leukaemia cells can infiltrate bones, causing deep bone pain that parents often mistake for normal growth-related discomfort.– If a child limps frequently or avoids walking, it could be a red flag. 3. Gum Swelling and Bleeding – leukaemia can cause gingival hyperplasia (gum overgrowth) and frequent bleeding of the gums.– This is often mistaken for poor dental hygiene or vitamin deficiencies. 4. Frequent Infections Without a Fever – While recurrent fevers are a well-known sign, some children may experience constant low immunity without developing noticeable fevers.– Persistent sinus infections or fungal infections unresponsive to antibiotics may indicate an issue with white blood cell function. 5. Abdominal Swelling Due to Organ Enlargement – leukaemia can lead to swelling of the liver and spleen, causing the belly to appear bloated.– It might be mistaken for dietary bloating or digestive issues. Hidden Causes and Risk Factors of Childhood Leukemia 1. Prenatal and Early-Life Exposures – Exposure to high levels of pesticides, benzene, or household chemicals during pregnancy has been linked to a higher risk.– Some studies suggest maternal stress and infections during pregnancy could influence fetal immune development, increasing susceptibility. 2. Links to Gut Microbiome – Researchers have found that imbalanced gut bacteria in early childhood may contribute to leukemia risk.– Children raised in extremely sterile environments with low exposure to microbes may have underdeveloped immune systems, leading to abnormal immune responses. 3. The Role of Hidden Genetic Mutations – While some genetic mutations are inherited, many leukemia-related mutations occur spontaneously in the womb and remain undetected until symptoms appear.– Some children may carry mutations in the PAX5 gene or ETV6 gene, increasing their risk of leukemia without a family history. 4. High-Risk Environmental Factors – Living near high-voltage power lines or prolonged exposure to electromagnetic radiation is being explored as a possible contributing factor.– Certain artificial food dyes and preservatives are also being studied for their potential effects on cellular DNA. Little-Known Facts About Treatment and Recovery 1. Some Forms of Childhood Leukemia Can Resolve Without Immediate Treatment – A rare condition called Transient Abnormal Myelopoiesis (TAM) in newborns with Down syndrome mimics leukemia but often disappears without treatment.– This has led researchers to explore natural immune mechanisms that might help combat leukemia in its early stages. 2. Immunotherapy May Replace Chemotherapy in the Future – CAR-T cell therapy, a revolutionary treatment, uses the child’s own immune cells to fight leukemia and is showing promising results with fewer long-term side effects than chemotherapy.– Some new trials are testing cancer vaccines that train the immune system to recognize leukemia cells early. 3. Chemo Brain Affects Children Differently – Many childhood leukemia survivors experience ‘chemo brain,’ leading to cognitive difficulties, but brain plasticity in children allows better recovery than in adults.– Cognitive therapy and omega-3 fatty acids are being studied for their role in improving brain function post-treatment. 4. Leukemia Cells Can “Hide” from Treatment – Some leukemia cells evade chemotherapy by entering a sleep-like state within bone marrow niches.– New treatments aim to ‘wake up’ these dormant cells before targeting them with drugs. 5. Survivors Have a Higher Risk of Second Cancers – Childhood leukemia survivors have a 4-6 times higher risk of developing a secondary cancer later in life due to previous chemotherapy and radiation exposure.– Long-term follow-ups and nutrient-rich diets are recommended to help mitigate this risk. Final Thoughts While childhood leukemia is a life-altering diagnosis, research continues to uncover hidden factors that influence its development, progression, and treatment. Parents and caregivers should remain vigilant about uncommon symptoms and seek early medical evaluation for persistent health issues. With the rapid advancement of targeted therapies and personalized medicine, the future holds hope for better survival rates and fewer long-term complications for young patients.
